
Dylan Knowles is a healthcare modeler and software engineer who helps government, business, and teams solve seemingly intractable problems. His core skill is weaving stories from evidence to inform strategy rather than simply providing metrics.
When simulation professionals think of modeling, they often imagine large-scale systems—healthcare networks, supply chains, airport operations, or logistics corridors. These models capture countless interactions, optimize resource flows, and guide strategic decisions.
Yet some projects demand that we shrink our perspective. When the system under study isn’t a city or a hospital but a single human being, the stakes and urgency feel profoundly different.
This is the story of how I applied predictive modeling in healthcare using AnyLogic to help support someone living with a Parkinsonian condition, creating a personalized medicine dosing simulation tool.
Contents:
- When it’s personal
- From sketch to personalized medication simulation
- From one patient to many
- Why AnyLogic?
- Key takeaways
When it’s personal
Our story begins with a change. Someone close to me was diagnosed with a Parkinsonian disorder and was prescribed levodopa three times a day. While this is standard practice, an individual’s response to the drug is highly personal. An amount that leads to good outcomes for some can be ineffective or cause extreme side effects in others.
The devil is in the details
Levodopa is the gold-standard medication used to treat conditions with impaired dopamine production or receptivity, like Parkinson’s disease. Despite its discovery over a century ago and widespread use for the last 50 years, levodopa’s fundamental challenges remain.
Levodopa has an extremely short half-life, which can cause highly unstable blood serum levels and rapid shifts between symptom relief and side effects. The body metabolizes it almost immediately, and only a tiny amount reaches its target deep in the brain.
Responses to the same dose and formulation can vary greatly between men and women, and factors such as diet, illness, stress, poor sleep, and menstrual cycles can significantly alter its effects. These complexities highlight the need for personalized medicine approaches to manage treatment more effectively. To design truly effective treatment strategies, we have to go beyond the data and account for the realities of daily living.
Dealing with everyday life

Levodopa is sensitive to day-to-day changes in an individual’s life. This requires us to consider real-world variables.
Sleep quality
Poor sleep often makes symptoms worse the next day. On low-sleep days, the same dose of levodopa could have noticeably weaker effects. Worse yet, the incorrect amount of levodopa can exacerbate sleep challenges, resulting in a feedback loop.
Meal timing
The drug competes with dietary protein for absorption. When taken around high-protein meals, its effectiveness drops. Recognizing this pattern highlights how meal composition and timing can directly influence how well a dose works.
Emotional stress
Stress can trigger tremors, exacerbate dyskinesia, and make symptoms less predictable, even when medication levels seem appropriate. It underscores how emotional and psychological states could significantly affect symptom control.
Read also: check out other cases of using predictive modeling in healthcare.
These observations reinforce a key truth about predictive modeling in healthcare: biology alone doesn’t tell the full story. Effective personalized medicine must consider lifestyle factors, daily routines, and patient attributes like gender and existing medications. Understanding this broader context is essential to designing treatment plans that work in the real world, not just on paper.
That’s when I began exploring how simulation could support personalized medicine planning.
From sketch to personalized medication simulation
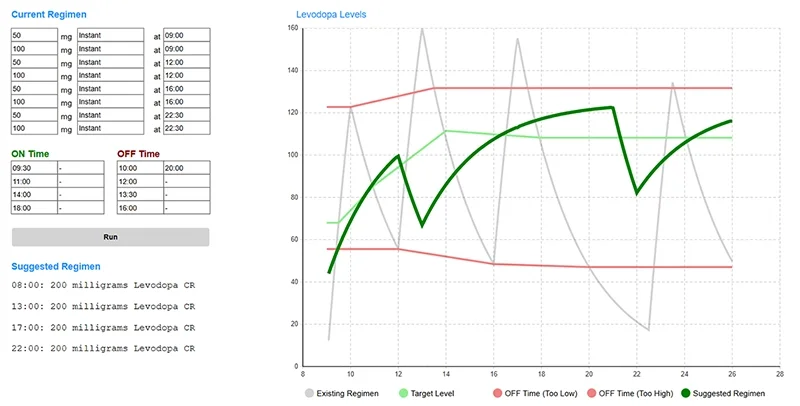
Levodopa is hard to get right. Rather than guessing, we turned to predictive modeling in healthcare by simulating personalized medication strategies. I began with a basic sketch of a system dynamics model of levodopa accumulation and decay. The pattern was clear: three evenly spaced doses weren’t enough.
Next, we quickly found a controlled-release formula, but its reported effectiveness varied considerably. Some doctors swore by it; others reported no benefit. This is when we brought in AnyLogic and began applying predictive modeling techniques.
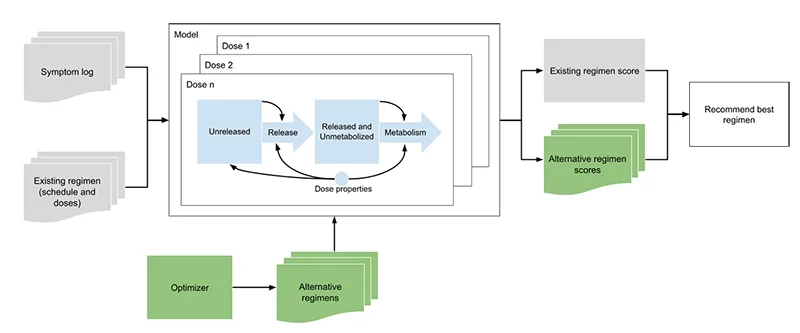
We developed a system dynamics model, made it runnable, and compared personalized medication strategies. From the results of an instant release simulation, we inferred that controlled release would help reach our target therapeutic window more reliably. By combining with instant release, we could get there faster.
Model and reality quickly met. Symptoms improved, but then came the crash, and midday exhaustion struck hard. The model indicated that even a 30-minute error in timing could drastically affect patient response.
To manage this complexity, we connected system dynamics with agent-based modeling and used AnyLogic’s optimizer to trial thousands of personalized medication strategies. This application of predictive modeling in healthcare tailored regimens to the individual patients rather than relying on average trends.
From one patient to many: scaling predictive modeling in healthcare
After three months of iteration, symptoms and side effects were well managed. It was a hopeful period after months of scrambling to find a workable solution.
The model was refined. Word spread. A member of the local Parkinson’s community asked if we could try the model with her. Once again, the personalized medicine simulation predicted results that led to symptom improvement; nausea and dyskinesia, in her case, became substantially more manageable.
Currently, we are in the process of studying options for scaling this predictive modeling approach in healthcare: a cloud-hosted backend, a lightweight web interface, and personalized medicine achieved in weeks instead of years.
This tool doesn’t just apply to Parkinson’s. The same approach may be used for other rare neurological conditions where data is sparse and specialists are rare. It can also be used for other tricky medications with highly personal responses.
Why AnyLogic?
This work would not have been possible without AnyLogic. We needed multimethod modeling capabilities, rapid deployment, and a way to embed a personalized medication optimizer into a scalable framework. Other tools would have required time-consuming integration. AnyLogic let us prototype and deploy quickly, making it ideal for predictive modeling in healthcare.
Key takeaways
Applying predictive modeling in healthcare to real-world personalized medicine taught us more than we expected:
- Speed matters. Going from sketch to functional simulation in days allowed us to respond when traditional care pathways could not.
- Simulation reveals insights. Even a simple model exposed the limitations of existing medication regimens—and made them addressable.
- Patients are active participants. Their direct feedback helped us improve the model and its recommendations, turning patients into empowered collaborators.
- Cloud enables access and personalization. Deploying the model online makes this technology useful not just for researchers but for real patients and clinicians at the point of care.
Thanks to simulation, one person avoided years of painful trial-and-error while personalizing their medication. This demonstrates the undeniable potential of predictive modeling in healthcare: delivering faster, more personalized, and data-driven decisions that improve patient outcomes when time, clarity, and precision matter most.
Simulation is no longer just for large systems—it’s for people, too.
To keep improving, the project needs data from people living with Parkinson’s disease or Parkinsonian conditions, including symptom journals and medication schedules. If you’re open to contributing or interested in participating in early trials, please get in touch.







